How it works
Optimize your healthcare workforce:
How it works
Optimize your healthcare workforce:
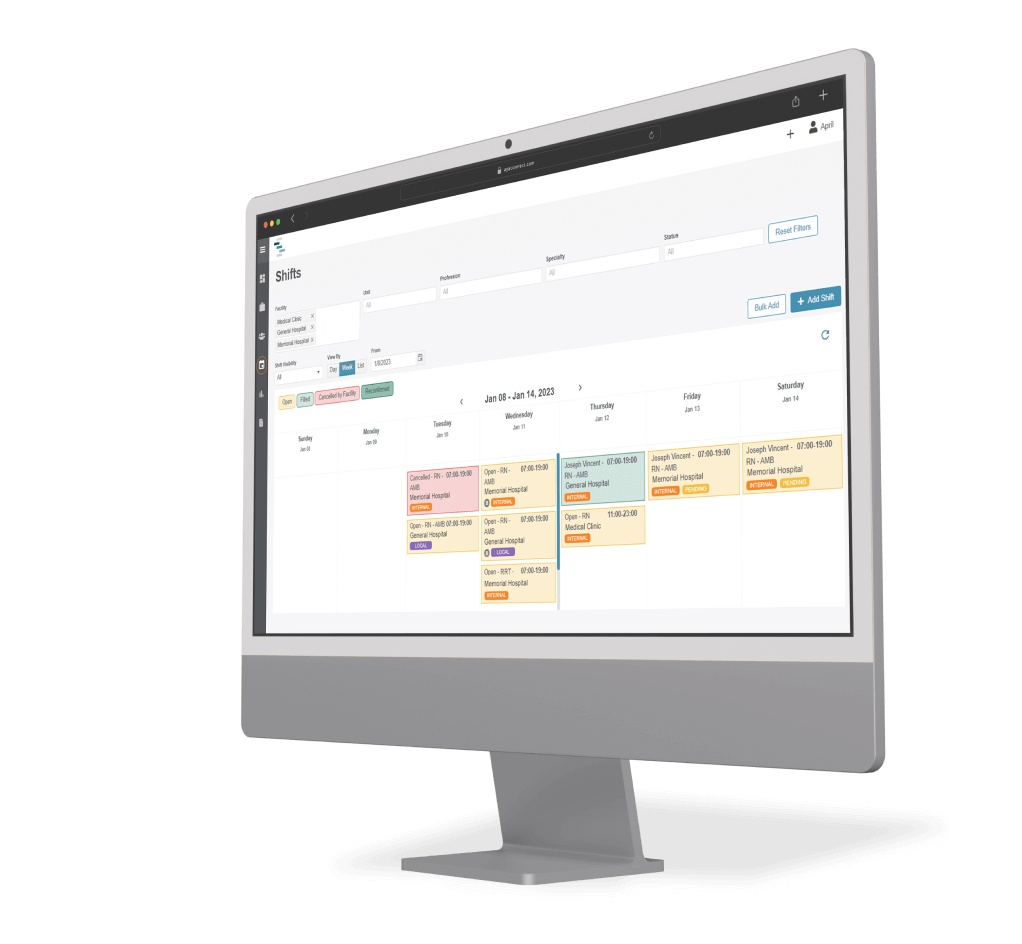
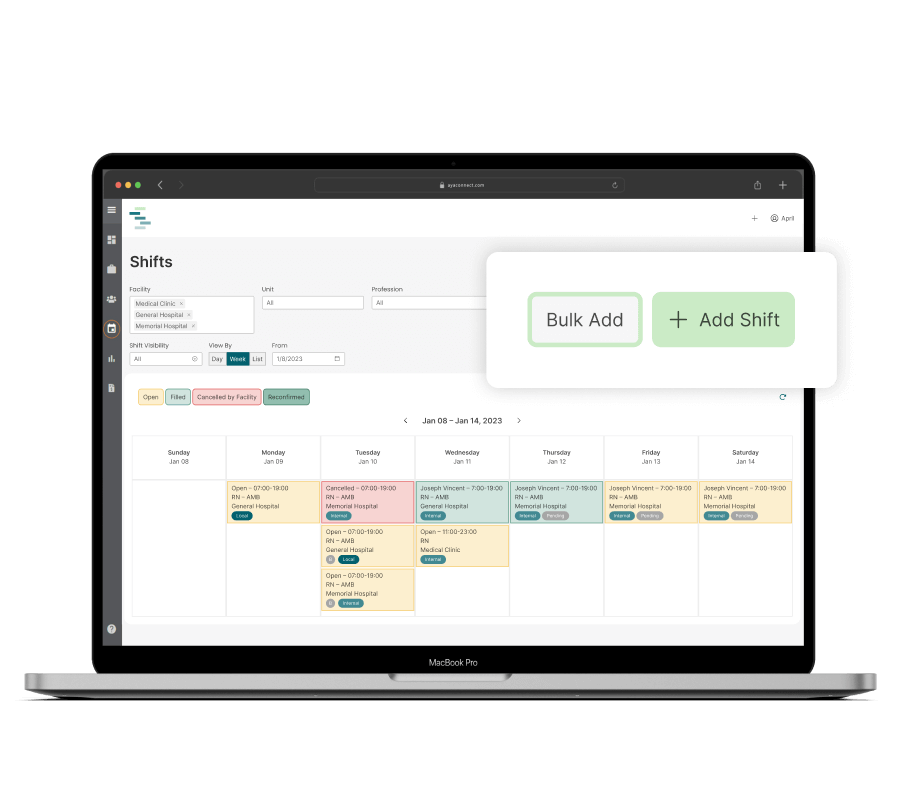
Post open shifts.
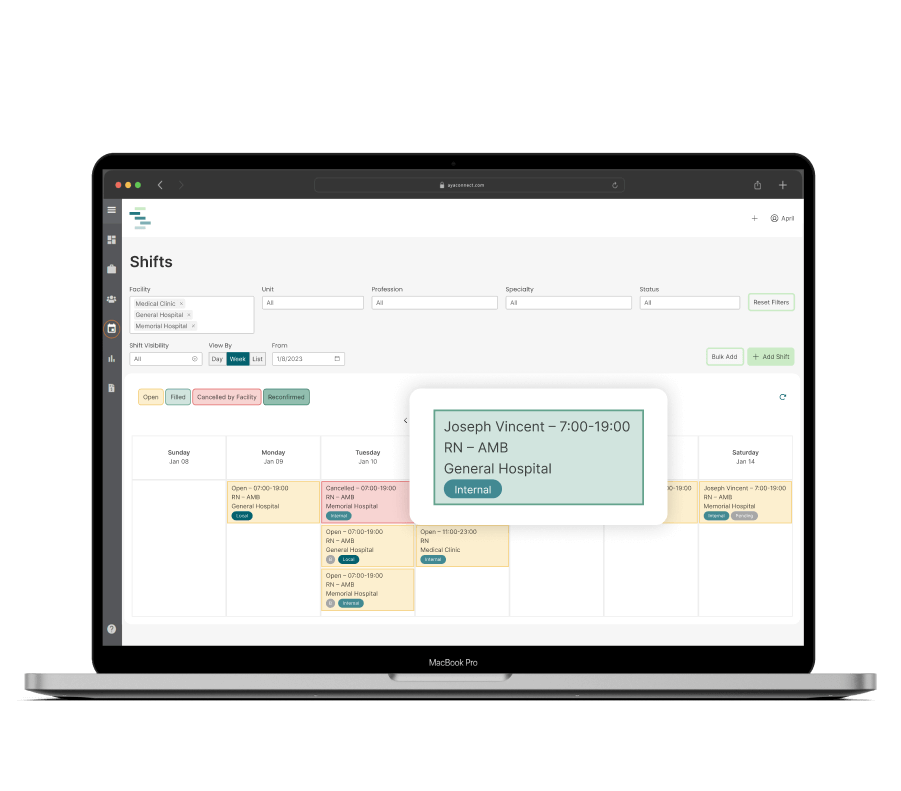
Mobilize your internal workers with app-based deployment and communications.
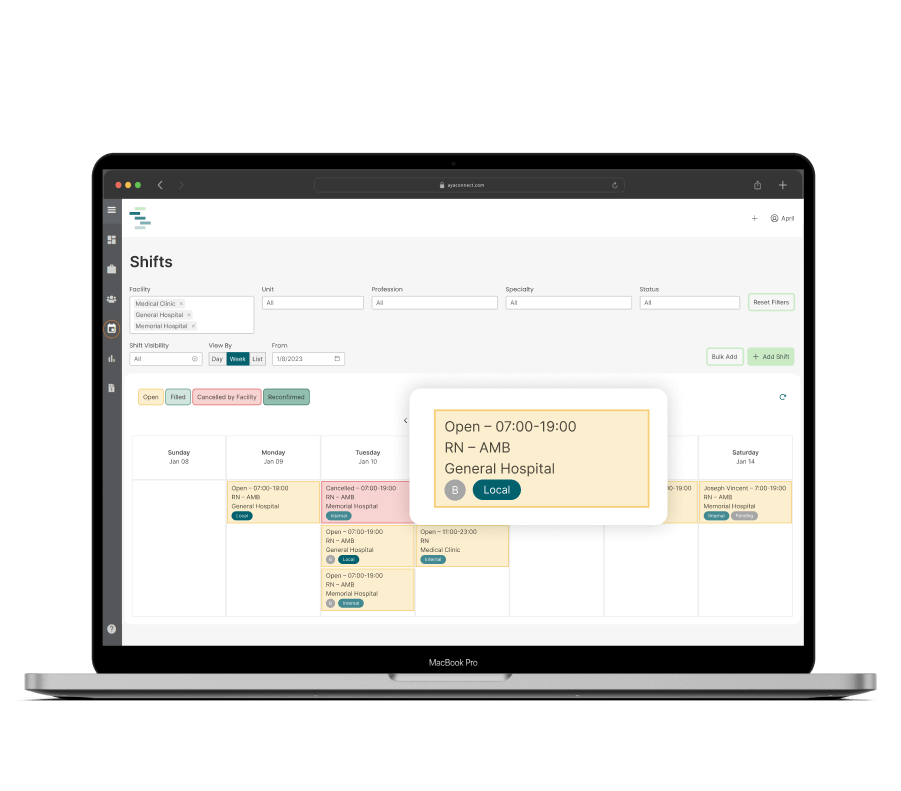
Expand your reach by streamlining your local agencies and gig workers on one platform.
Flexible. Fast. Efficient.
Get shifts filled with our on-demand clinical labor platform. Designed for flexibility, easily manage shifts among your internal resource pool and external PRN staff. Standard integrations and mobile app capabilities automate workflows and provide real-time notifications to fill open needs quickly.
Need recruitment assistance? Get your pool started by sourcing from the largest clinical talent pool in the U.S.
Register to get a demoEffective float pool management to reduce premium labor costs
App-based deployment with real-time notifications
Release jobs to internal staff, then to external workers
AI tools forecast gaps to optimize staffing
System integrations automate workflows and sync data
Quick implementation and rapid adoption
Customized reporting and robust analytics

Harnessing workforce AI for optimal staffing
Shifts leverages Workforce AI to accurately forecast patient volume and generate optimal staffing recommendations. With a consolidated view of staffing across units and full visibility into every resource pool, sophisticated algorithms inform systems on how to effectively distribute internal resources and plan alternative schedules. We’re here to help you successfully face today and whatever tomorrow brings.